For most plans, open enrollment season takes place in November or December. Now is an ideal time to consider how compliance rules impact the enrollment process and prepare for a successful open enrollment season.
Key Enrollment Periods
Employees generally have three opportunities to enroll in or change their benefits:
- Initial Enrollment: Newly eligible employees can enroll as they become eligible, ahead of the next open enrollment period.
- Open Enrollment: All eligible employees can elect or modify their plan choices before the annual renewal date.
- Special Enrollment: Individuals can enroll or make changes due to specific life events, like marriage, birth, or job loss.
The Importance of Open Enrollment
Several compliance factors necessitate an annual open enrollment period: 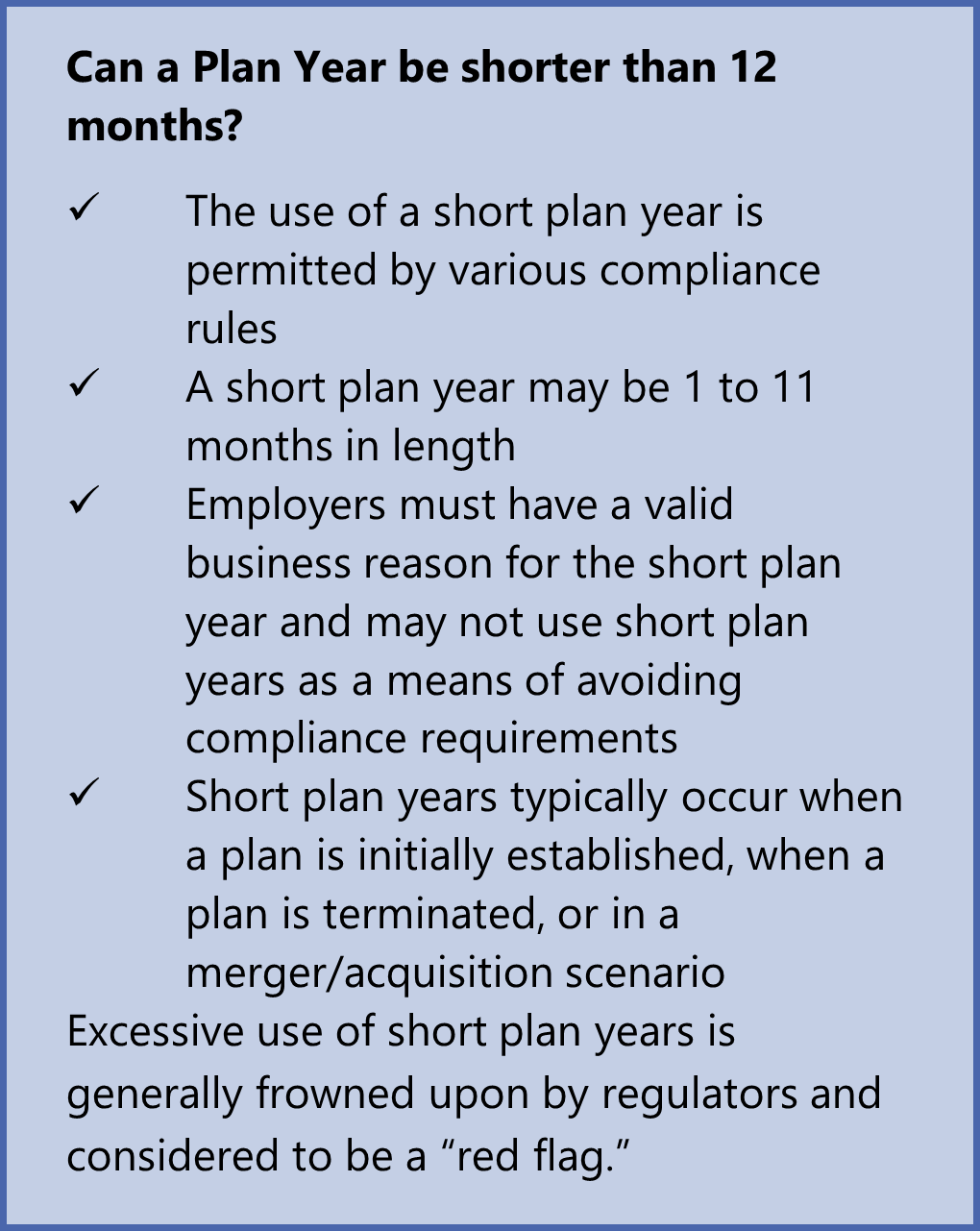
Plan Year Requirements: ERISA and Section 125 mandate that plan years cannot exceed 12 months, requiring annual renewal.
Cafeteria Plan Elections: Cafeteria plan elections must be made before the coverage period begins, with limited exceptions for special enrollment or initial enrollment within 30 days of hire.
ACA Compliance: The Affordable Care Act requires large employers to offer affordable health coverage to full-time employees, making open enrollment a crucial time to assess plan affordability.
The Role of Plan Documents
Plan documents, including the Summary Plan Description (SPD) and Summary of Material Modifications (SMM), outline eligibility requirements, enrollment procedures, and other important details. Adhering to these documents is a fiduciary responsibility under ERISA.
Responsibilities of Key Players
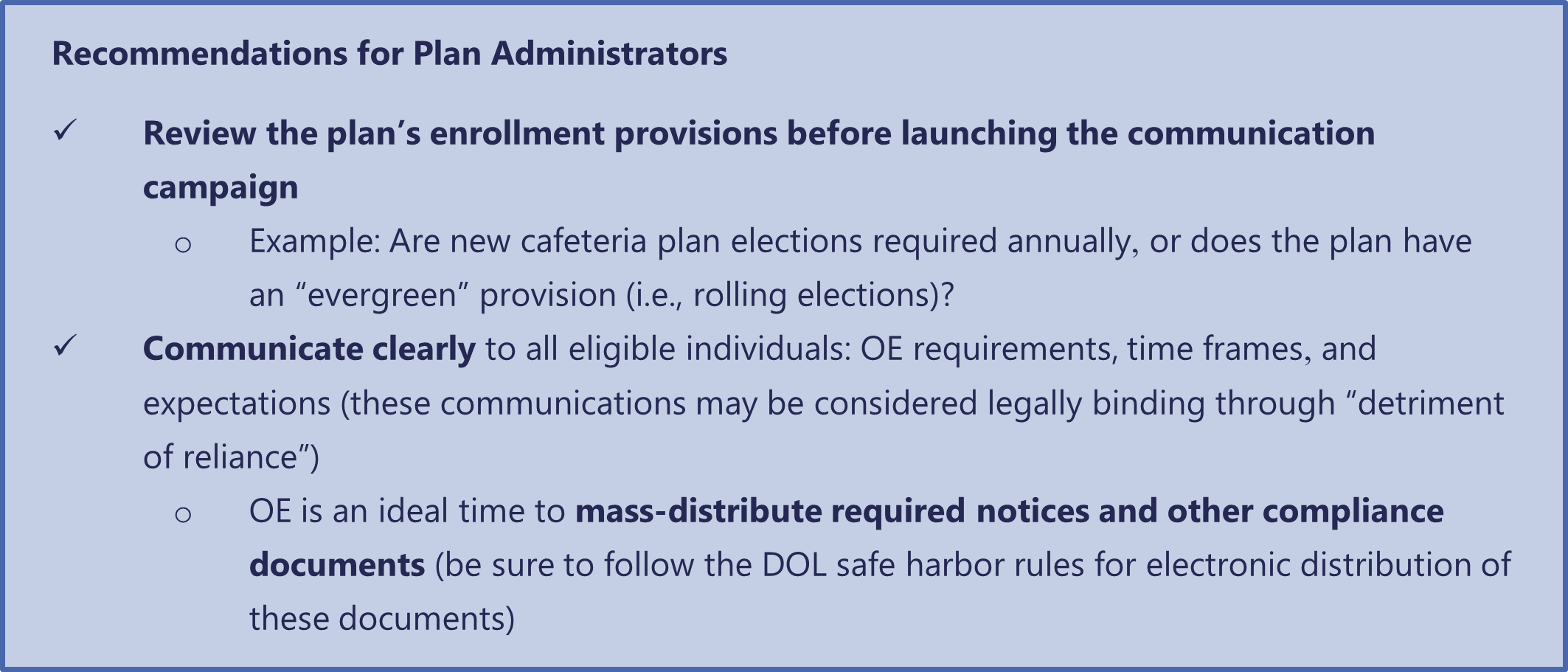
Plan Administrator: Oversees the entire enrollment process, ensuring compliance with regulations and plan documents.
Insurer or Third-Party Administrator (TPA): Provides guidance on enrollment procedures and may have specific guidelines that employers must follow.
Updating Plan Documents
When significant changes occur to a benefit plan, plan documents must be updated to reflect the changes. This includes distributing updated SPDs or SMMs to employees.
Inclusive Open Enrollment
It's essential to remember that all eligible employees, including those on COBRA or FMLA leave, should have access to open enrollment materials and opportunities.
Conclusion
Navigating the complexities of open enrollment requires a thorough understanding of compliance rules and careful planning. By adhering to regulations and providing clear and timely communication to employees, employers can ensure a successful open enrollment process.





